Georgia Medicaid program with work requirement off to slow start even as thousands lose coverage
ATLANTA (AP) — Georgia Gov. Brian Kemp signed paperwork creating a new state health plan for low-income residents to much fanfare at the state Capitol three years ago.
But public health experts and advocates say since it launched on July 1, state officials appear to be doing little to promote or enroll people in the nation’s only Medicaid program that makes recipients meet a work requirement.
The Georgia Department of Community Health, which has projected up to 100,000 people could eventually benefit from Georgia Pathways to Coverage, had approved just 265 applications by early August.
“If we’re talking about directed outreach to the population that would most likely be eligible and interested, I haven’t seen anything,” said Harry Heiman, a health policy professor at Georgia State University.
 Local governments are spending billions of pandemic relief funds, but some report few specifics
Local governments are spending billions of pandemic relief funds, but some report few specifics
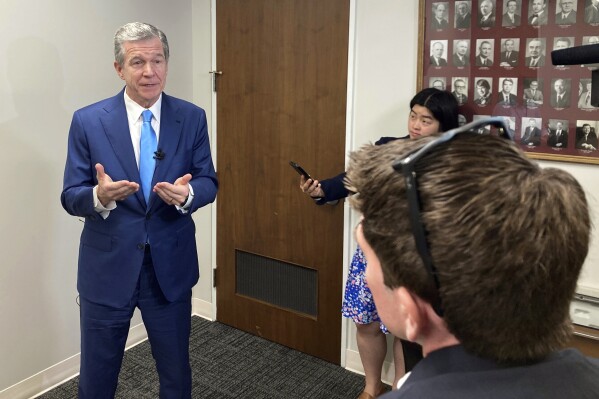 North Carolina’s governor visits rural areas to promote Medicaid expansion delayed by budget wait
North Carolina’s governor visits rural areas to promote Medicaid expansion delayed by budget wait
 Feds raise concerns about long call center wait times as millions dropped from Medicaid
Feds raise concerns about long call center wait times as millions dropped from Medicaid
Heiman and other experts say the program’s slow start reflects fundamental flaws missing from Medicaid expansions in other states, including the extra burden of submitting and verifying work hours. And some critics note it’s happening just as the state, as part of a federally mandated review, is kicking tens of thousands of people off its Medicaid rolls — at least some of whom could be eligible for Pathways.
“We’ve chosen a much more complicated and lengthy process that will take a long time even for the few folks who get coverage,” said Laura Colbert, executive director of the advocacy group Georgians for a Healthy Future.
The Biden administration has already tried to revoke Georgia’s Medicaid plan once and will be monitoring it, so any missteps could have broader consequences. They could also hamper future efforts by Republicans to make Medicaid eligibility dependent on work.
A spokesman for the governor’s office, Garrison Douglas, said enrollment would grow as applications continue to be reviewed.
“While the federal government initiated and dictated a process for re-determining the qualifications of traditional Medicaid recipients, Georgia is the only state in the country simultaneously offering a new pathway to healthcare coverage and opportunity,” he said in a statement.
The state’s department of community health said it was engaging stakeholders, community partners and others to help get the word out about the program. It did not provide details about that effort.
“There’s still some more work that we have to do for Pathways,” Lynnette Rhodes, executive director of DCH’s Medical Assistance Plans division, said at a meeting this month. “But overall...the program is working.”
The state launched Pathways just as it began a review of Medicaid eligibility following the end of the COVID-19 public health emergency. Federal law prohibited states from removing people from Medicaid during the three-year emergency.
Georgia has already cut more than 170,000 adults and kids from Medicaid and is expected to remove thousands more as the yearlong review of all 2.7 million Medicaid recipients in the state continues. Nationwide, more than a million people have been dropped from Medicaid, most for failing to fill out paperwork.
The department of community health said it delayed the reevaluations of 160,000 people who were no longer eligible for traditional Medicaid but could qualify for Pathways to help them try to maintain health coverage. It was not immediately clear whether the state reached out to those people and helped guide them to apply for Pathways.
“From what we have seen thus far, they are not doing anything affirmatively to get these people enrolled in Pathways,” said Cynthia Gibson, an attorney with the Georgia Legal Services Program who helps people obtain Medicaid coverage.
In contrast, Oklahoma officials implementing a voter-approved expansion of Medicaid in 2021 moved people in existing state insurance programs directly into the expansion pool without the need for a new application, according to the Oklahoma Health Care Authority. Nearly 100,000 people were enrolled in the expanded program within days of its launch.
“States have a lot of tools that they can use to help make this process go more smoothly,” said Lucy Dagneau, an advocate for Medicaid expansion with the American Cancer Society Cancer Action Network.
Oklahoma and 39 other states have expanded Medicaid eligibility to nearly all adults with incomes up to 138% of the federal poverty level, $20,120 annually for a single person and $41,400 for a family of four. None of those states require recipients to work in order to qualify.
That broader Medicaid expansion was a key part of President Barack Obama’s health care overhaul in 2010, but many Republican governors, including Kemp, rejected it. In addition to imposing a work requirement, Pathways limits coverage to able-bodied adults earning up to 100% of the poverty line — $14,580 for a single person or $30,000 for a family of four.
Kemp has argued full expansion would cost too much money. State officials and supporters of Pathways say the work requirement will also help transition Medicaid recipients to better, private health insurance, and working, studying or volunteering leads to improved health.
“I’m excited we’re moving forward in this direction,” said Jason Bearden, president of CareSource Georgia, one of the state’s Medicaid health plans. “This is good progress.”
Critics say many low-income people work informal jobs and have fluctuating hours that will make it hard for them to document the required 80 hours a month of work, volunteer activity, study or vocational rehabilitation. They also blast the lack of an exemption to the work requirement for parents and other caregivers.
For Amanda Lucas, the work requirement is insurmountable right now.
Lucas said she had no idea Pathways started in July, but even if she did, she would not qualify because she has to take care of her 84-year-old father in Warner Robins, a city about 100 miles (160 km) south of Atlanta. He had a stroke and needs her to buy groceries, make food, pick up prescriptions, pay bills and manage myriad other tasks, she said.
With risk factors for skin cancer, she worries about living without health insurance.
“I try to keep an eye on my own moles,” she said. “I’m increasingly anxious because I’m 46.”
Disclaimer: The copyright of this article belongs to the original author. Reposting this article is solely for the purpose of information dissemination and does not constitute any investment advice. If there is any infringement, please contact us immediately. We will make corrections or deletions as necessary. Thank you.




